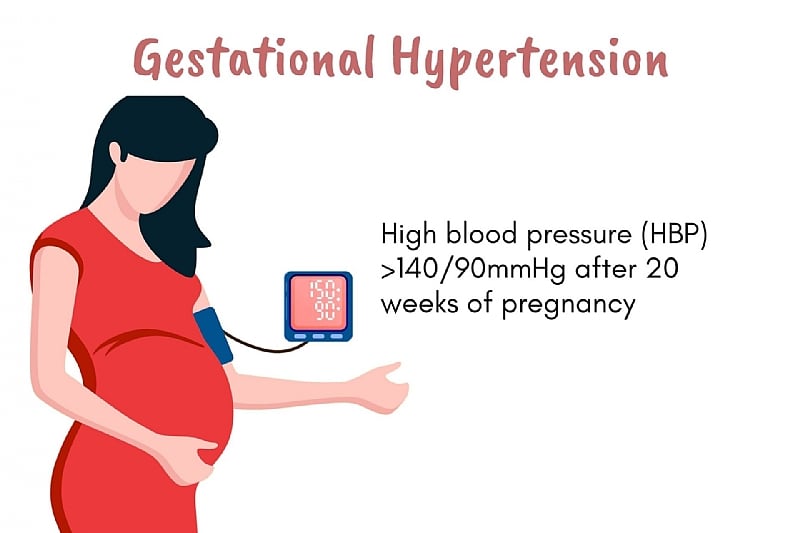
Gestational hypertension, a prevalent pregnancy-specific condition, emerges after 20 weeks of gestation in women with previously normal blood pressure. Defined by elevated blood pressure exceeding 140/90 mmHg without significant proteinuria or organ dysfunction, it necessitates meticulous monitoring and intervention to safeguard both maternal and fetal well-being. The diagnosis hinges on the resolution of hypertension within 12 weeks postpartum, differentiating it from chronic hypertension. This condition carries significant implications for both present and future maternal health, requiring a comprehensive understanding of its definition, diagnostic criteria, management, and long-term risks.
Gestational hypertension falls within the spectrum of hypertensive disorders of pregnancy, alongside preeclampsia, chronic hypertension, and preeclampsia superimposed on chronic hypertension. Accurate differentiation is crucial for tailored management strategies. Unlike preeclampsia, gestational hypertension lacks proteinuria and signs of organ damage. Chronic hypertension, on the other hand, precedes pregnancy or is diagnosed before 20 weeks. The diagnostic process involves careful blood pressure measurement, excluding white coat hypertension, and evaluating for preeclampsia symptoms. Laboratory tests assess urine protein, platelet count, liver enzymes, and kidney function to eliminate other potential causes like glomerulonephritis or endocrine disorders.
Clinical management of gestational hypertension hinges on the severity of blood pressure elevation. Severe hypertension (above 160/110 mmHg) mandates immediate hospitalization and often necessitates delivery to mitigate maternal risks like stroke or organ damage. Non-severe cases can be managed on an outpatient basis with regular blood pressure and laboratory monitoring. Patients receive education on preeclampsia symptoms and are advised to avoid strenuous activities. Antihypertensive medications like labetalol, nifedipine, and methyldopa are reserved for persistently high or rapidly increasing blood pressure. Fetal well-being is closely monitored using non-stress tests, biophysical profiles, and ultrasounds to assess growth and amniotic fluid levels.
The optimal delivery timing in gestational hypertension aims for term (37-39 weeks) if maternal and fetal conditions permit. However, uncontrolled blood pressure or emerging complications may necessitate earlier delivery. Postpartum, blood pressure typically normalizes within 12 weeks. Despite this resolution, women with gestational hypertension face an elevated risk of developing chronic hypertension and cardiovascular disease later in life, underscoring the importance of long-term follow-up and preventative measures.
While most cases resolve postpartum, gestational hypertension carries significant long-term maternal health risks, including hypertension, ischemic heart disease, and stroke. The condition also increases the likelihood of recurrence in subsequent pregnancies. Prophylactic low-dose aspirin, initiated early in pregnancy, can mitigate this risk. Perinatal outcomes in non-severe gestational hypertension are generally positive, with low rates of preterm birth and growth restriction. However, severe gestational hypertension elevates the risk of adverse outcomes, including preterm delivery, small-for-gestational-age infants, and placental abruption. This reinforces the need for vigilant blood pressure control and proactive management.
In summary, gestational hypertension, defined as new-onset hypertension after 20 weeks gestation without proteinuria or organ dysfunction, represents a significant pregnancy complication requiring meticulous monitoring and management. Accurate diagnosis, distinguishing it from other hypertensive disorders, is crucial for appropriate interventions. Management strategies are tailored to the severity of hypertension, focusing on controlling blood pressure and ensuring fetal well-being. While often resolving postpartum, gestational hypertension increases the long-term risk of cardiovascular disease in women. Early identification, careful management, and postpartum surveillance are essential for optimizing both maternal and fetal outcomes, making gestational hypertension a critical focus in prenatal and ongoing healthcare.