Thyroid cancer, a malignancy originating in the thyroid gland, has witnessed a concerning global surge in incidence, particularly among women. India reflects this trend, with thyroid cancer increasingly featuring among the top cancers affecting women. While heightened awareness has fostered earlier detection, several myths persist, hindering timely diagnosis and appropriate management. Debunking these misconceptions is crucial for effective disease control and improved patient outcomes.
One prevalent myth portrays thyroid cancer as a rare occurrence. Contrary to this belief, thyroid cancer’s incidence has been steadily increasing worldwide, significantly affecting women in India. This rise is partly attributable to improved diagnostic tools like ultrasound, enabling better detection of smaller nodules. However, lifestyle and environmental factors also contribute to the increasing prevalence. Recognizing thyroid cancer as a prevalent disease, particularly among women, underscores the importance of regular screening and medical consultations.
Another misconception confines thyroid cancer primarily to older adults. While age remains a risk factor, thyroid cancer increasingly affects younger demographics, including women in their 20s, 30s, and 40s. Specific subtypes, notably papillary thyroid cancer, exhibit a higher incidence in younger women. Therefore, considering age alone as a determinant for risk assessment can be misleading. Vigilance and proactive healthcare are essential for all age groups, especially women.
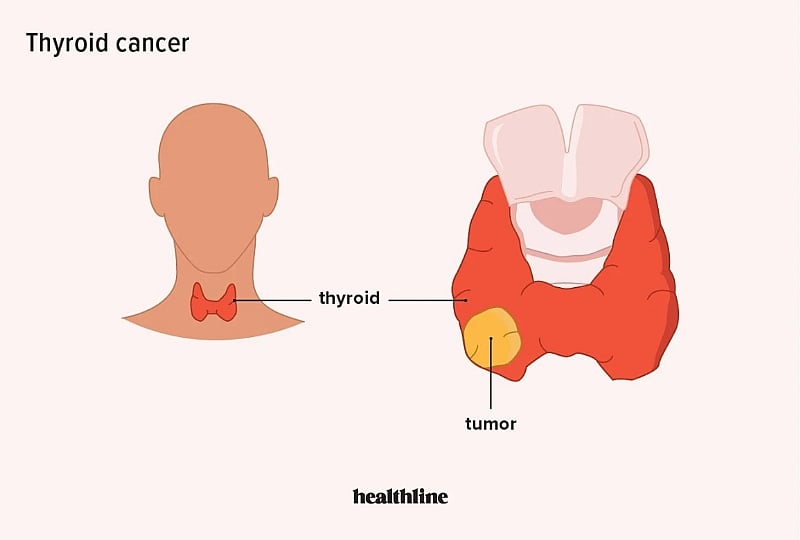
A common fear associates any neck lump with cancer. While a neck lump can be indicative of thyroid cancer, the majority of thyroid nodules are benign. However, differentiating benign from malignant nodules requires medical evaluation, including ultrasound examination and potentially a biopsy. Self-examination of the neck (neck checks) and timely consultation with a physician are crucial steps in assessment and diagnosis. Dismissing a neck lump as harmless can lead to delayed diagnosis and potentially adverse consequences.
The notion that thyroid cancer always presents with noticeable symptoms is also misleading. Early-stage thyroid cancer often remains asymptomatic or exhibits subtle, easily overlooked symptoms. Hoarseness, difficulty swallowing, or neck swelling may not manifest until the disease progresses. Waiting for overt symptoms can delay diagnosis and compromise treatment effectiveness. Regular screening and prompt medical attention for any suspicious signs are vital.
Finally, the misconception that thyroid cancer treatment invariably leads to lifelong complications is unfounded. Modern treatment modalities, including surgery, radioiodine therapy, and hormone replacement therapy, offer excellent outcomes for most patients. Contrary to outdated beliefs, patients typically retain their voice and regain their strength after treatment. Quality of life post-treatment is generally excellent with appropriate medical follow-up and management.
In conclusion, thyroid cancer, despite its increasing incidence, carries a positive prognosis when detected and treated early. Addressing misconceptions about the disease, promoting awareness, encouraging self-checks, and ensuring timely medical evaluation are vital steps in improving patient outcomes. Ignoring warning signs, especially a painless neck lump, can delay diagnosis and compromise treatment success. Thyroid cancer, when managed effectively, allows patients to lead healthy and fulfilling lives. The emphasis should remain on early detection, prompt intervention, and ongoing medical care to maximize positive outcomes.