Glioblastoma, an aggressive and challenging brain tumor, has long been a source of despair for patients and medical professionals alike. Its rapid growth and infiltration into surrounding brain tissue make complete surgical removal extremely difficult, and recurrence is common. Traditional treatments, involving surgery, radiation, and chemotherapy, have often yielded limited success. The unique nature of glioblastoma, residing within the complex and vital organ of the brain, demands a nuanced approach that goes beyond simply removing or shrinking the tumor. Treatment must delicately navigate the brain’s intricate functionalities, preserving essential cognitive and motor skills. This very complexity, however, has propelled remarkable innovations in neuroscience and oncology, offering a renewed sense of hope in the fight against this formidable disease.
A significant advancement in glioblastoma treatment is the shift towards personalized medicine. Recognizing that each tumor possesses a unique molecular fingerprint, researchers are moving away from standardized protocols. By analyzing the tumor’s genetic makeup, specialists can tailor treatment strategies to target the specific vulnerabilities of individual cases. This approach utilizes targeted medications and therapies designed to maximize effectiveness based on the patient’s unique tumor biology. This personalized strategy represents a significant departure from the one-size-fits-all approach and offers a more precise and potentially more effective way to combat glioblastoma.
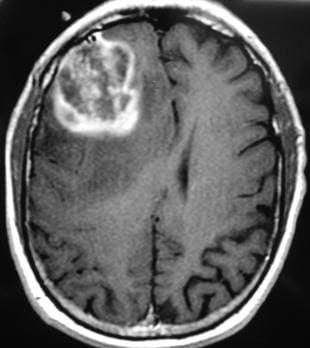
Surgical interventions for glioblastoma have also undergone a dramatic transformation. While surgery remains a cornerstone of treatment, cutting-edge techniques like Intraoperative MRI, Neuro-navigation, and Awake Brain Surgery have revolutionized the field. These technologies allow surgeons to map critical brain areas with unprecedented precision, minimizing the risk of damage to vital functions such as speech, vision, and movement. As a result, patients experience improved quality of life post-surgery, and in certain cases, more extensive tumor removal becomes possible, offering a better chance at controlling the disease.
Radiation therapy plays a crucial role in glioblastoma treatment, especially given the difficulty of achieving complete tumor resection through surgery. Radiation targets residual tumor cells left behind after surgery, effectively delaying recurrence and improving patients’ quality of life. Even in cases where complete surgical removal seems achievable, adjuvant radiation therapy is vital for eradicating microscopic tumor cells that may remain in the surrounding tissue. Modern radiation techniques, including image-guided radiotherapy (IGRT) and magnetic resonance imaging (MRI), allow for precise targeting of tumor cells, minimizing damage to healthy brain tissue and reducing side effects. The combination of radiation with chemotherapy drugs like Temozolomide further enhances the effectiveness of treatment by sensitizing tumor cells to radiation.
Immunotherapy, a revolutionary approach harnessing the body’s own immune system to fight cancer, holds immense promise for glioblastoma treatment. While still in its early stages of development for this specific cancer, immunotherapy aims to train the immune system to recognize and attack the tumor as a foreign invader. Experimental vaccines, T-cell therapies, and checkpoint inhibitors are currently being investigated for their potential in treating glioblastoma. This approach represents a paradigm shift, moving away from external attacks on the tumor to empowering the body’s internal defense mechanisms.
Artificial intelligence (AI) and machine learning are emerging as powerful tools in the fight against glioblastoma. From predicting patient responses to treatment to mapping tumor progression, AI is transforming the landscape of diagnosis and care. These technologies assist doctors in making more informed and rapid decisions, leading to fewer invasive procedures and more proactive, personalized treatment plans. Even in India, leading institutions are integrating AI into radiology and diagnostics, enhancing the ability to detect subtle changes, assess treatment effectiveness, and tailor care pathways, optimizing treatment strategies and improving patient outcomes. Though glioblastoma remains a formidable adversary, the convergence of these advancements in treatment, technology, and understanding offers a beacon of hope in the ongoing battle against this challenging disease. The evolution from a sense of despair to one of empowered action is evident in the longer survival times, improved recoveries, and the increasing awareness surrounding brain malignancies. Continued research and open communication about this complex disease are crucial in fostering hope and driving progress towards a future where glioblastoma is no longer a terminal diagnosis, but a battle we are increasingly equipped to win.