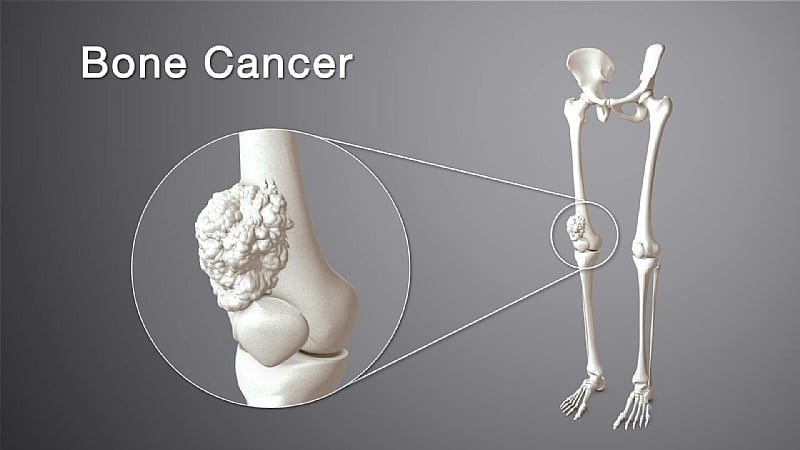
Bone cancer, a relatively rare yet aggressive disease, predominantly affects children and adolescents during periods of rapid bone growth, typically around the knees and upper arms. The diagnosis presents a significant emotional and physical strain on both the young patient and their family, who must grapple with complex decisions regarding treatment, surgery, and the arduous journey of recovery. Historically, the standard approach to bone cancer in a limb involved radical surgical removal of the affected bone segment, often culminating in amputation if the tumor was extensive or situated near vital structures. Survival was paramount, even at the expense of mobility. However, advancements in medical technology and surgical planning have ushered in a new era of limb-salvage procedures, offering a less drastic alternative for eligible patients. One such technique, known as extracorporeal irradiation (ECI), is steadily gaining recognition as a viable option for preserving limbs in young individuals battling bone cancer.
ECI involves a meticulous process of surgically removing the bone segment containing the tumor. This excised portion is then subjected to a high dose of radiation outside the body (extracorporeal) to eradicate any residual cancer cells. The precision of this radiation treatment is crucial; the objective is to completely eliminate cancerous cells while preserving the structural integrity of the bone. Following irradiation, the sterilized bone segment is reimplanted into its original location and securely affixed using specialized surgical hardware. The advantage of utilizing the patient’s own bone is the seamless reintegration into the skeletal structure, eliminating the need for artificial implants and the associated risks of rejection or complications. This method sidesteps the challenges of finding a suitable donor and the immunological complexities involved in transplantation.
The suitability of ECI is contingent upon several factors. Ideally, the tumor should be localized, without evidence of metastasis, and the patient should demonstrate a positive response to chemotherapy. The tumor’s location also plays a critical role; it must be surgically accessible without jeopardizing surrounding nerves or vital structures. In the hands of experienced surgical oncologists, ECI has demonstrated promising outcomes. Children who undergo this procedure often exhibit good functional recovery in the months following surgery, and long-term follow-up studies have shown encouraging results, particularly when the cancer is detected and treated early. The success of ECI hinges on a combination of factors, including meticulous surgical technique, precise radiation delivery, and a multidisciplinary approach involving oncologists, surgeons, and rehabilitation specialists.
The implications of limb salvage for a child extend far beyond the physical realm. Limb loss can have profound psychological and social consequences, impacting a child’s self-image, ability to participate in activities, and overall quality of life. ECI, by preserving the limb, mitigates these challenges, allowing children to maintain a sense of normalcy and avoid the emotional burden associated with amputation. While the physical recovery process remains demanding, the psychological benefits of limb preservation contribute significantly to a child’s overall well-being. Children, with their inherent resilience, often recover more quickly than adults, and many are able to resume their daily routines without significant adaptations following rehabilitation.
The growing interest in limb-salvage techniques like ECI underscores a paradigm shift in pediatric oncology. The focus has expanded beyond mere survival to encompass a broader consideration of the patient’s quality of life. Medical professionals now prioritize not only eradicating the disease but also ensuring that the child can thrive physically, emotionally, and socially after treatment. This shift in perspective reflects a deeper understanding of the long-term implications of cancer treatment and the importance of preserving function and minimizing disability.
With increasing awareness and expertise in ECI, more hospitals are training surgical teams in this specialized procedure, making it accessible to a wider range of patients. While not a universal solution, ECI offers a valuable alternative for select children diagnosed with bone cancer, transforming a narrative of loss into one of preservation and hope. For families facing the daunting challenges of a bone cancer diagnosis, ECI provides a beacon of hope, offering a path towards recovery without the permanent physical and emotional scars of amputation. It empowers families to navigate the complexities of cancer treatment with a renewed sense of optimism, knowing that their child has a chance to retain their limb and regain their quality of life. The availability of ECI signifies not only a medical advancement but also a profound shift in the approach to pediatric cancer care, prioritizing both survival and the preservation of a child’s future.