Glaucoma, often referred to as the “silent thief of sight,” is a progressive eye disease characterized by damage to the optic nerve, the vital link transmitting visual information from the eye to the brain. This damage is typically caused by elevated intraocular pressure (IOP), the pressure within the eye. The insidious nature of glaucoma lies in its often asymptomatic early stages. By the time noticeable vision changes occur, such as peripheral vision loss or seeing halos around lights, significant and often irreversible damage has already taken place. This underscores the crucial importance of regular eye exams for early detection, particularly for individuals at higher risk.
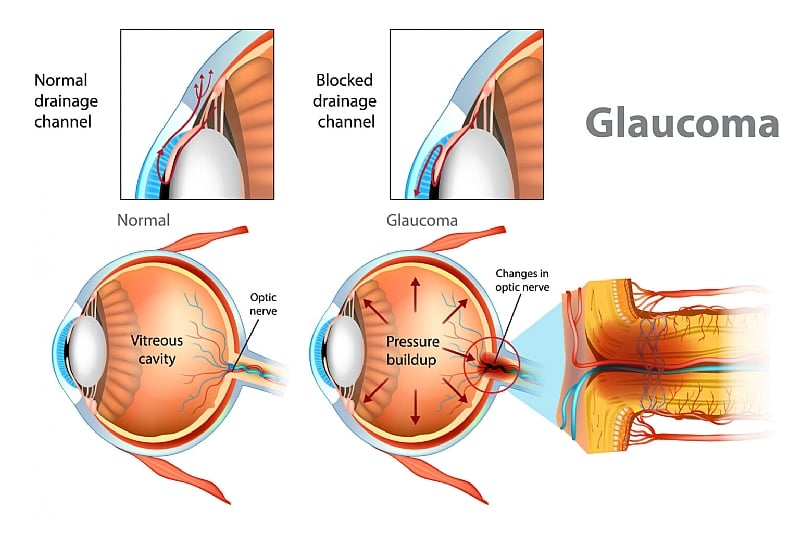
The aqueous humor, a clear fluid that nourishes and cleanses the eye’s internal structures, plays a central role in glaucoma. Normally, this fluid circulates continuously, maintaining a healthy IOP. However, in glaucoma, the drainage system for the aqueous humor becomes compromised, leading to fluid buildup and increased pressure. This elevated IOP can damage the delicate optic nerve fibers, leading to the formation of blind spots and, if left untreated, eventual blindness. The severity and progression of glaucoma vary, with different types categorized by their speed of onset and associated symptoms.
While lifestyle factors are not generally considered direct causes of glaucoma, certain triggers can exacerbate the condition or precipitate an acute attack in susceptible individuals. These triggers include extended periods in dark environments, pupil dilation, and stress. In particular, acute angle-closure glaucoma, a less common but more aggressive form of the disease, can progress rapidly, often accompanied by alarming symptoms such as severe eye pain, nausea, redness, and blurred vision. The intensity of these symptoms tends to correlate with the degree of IOP elevation.
Regular comprehensive eye exams are crucial for detecting glaucoma early, before significant vision loss occurs. The recommended frequency of these exams depends on individual risk factors. For those at low risk, exams are typically advised every 2-4 years before age 55, every 1-3 years between 55 and 64, and every 1-2 years after age 65. However, individuals at higher risk, including those with a family history of glaucoma, those of African, Asian, or Hispanic descent, individuals with a history of steroid use, or those who have experienced eye injuries, should undergo more frequent screenings, typically every 1-2 years.
Early detection is paramount in managing glaucoma effectively. While the disease can’t be cured, its progression can be slowed or halted, preserving remaining vision. Treatment options vary depending on the type and severity of glaucoma but often involve medications to lower IOP, laser procedures to improve aqueous humor drainage, or surgery to create new drainage pathways. Regular monitoring and adherence to the prescribed treatment plan are essential for successful long-term management. A glaucoma diagnosis doesn’t necessarily mean an immediate drastic change in lifestyle. With appropriate treatment and diligent care, many individuals with glaucoma can maintain a normal, active life.
Although early-stage glaucoma often presents no noticeable symptoms, certain warning signs should prompt immediate consultation with an eye care professional. These include blurred vision, difficulty focusing, eye redness, eye pain or pressure, nausea or vomiting associated with severe eye pain, halos around lights, and gradual loss of peripheral vision, sometimes described as “tunnel vision.” While these symptoms may not always indicate glaucoma, they warrant prompt evaluation to determine the underlying cause and initiate appropriate treatment if necessary. Early intervention is key to minimizing the impact of glaucoma and preserving vision.