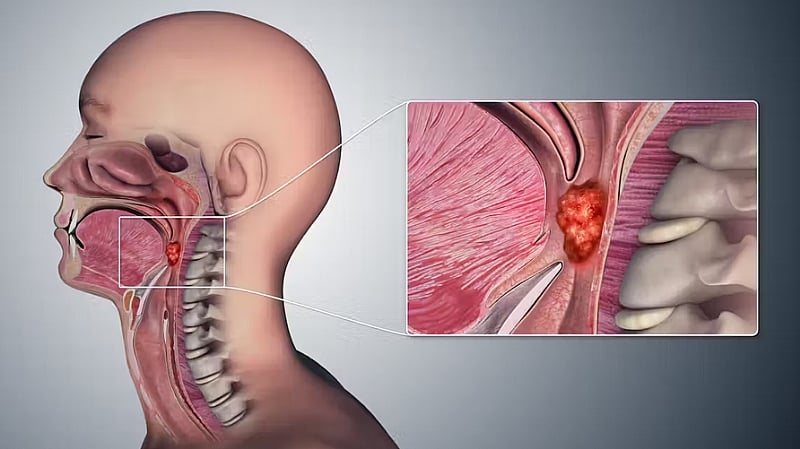
The landscape of cancer prevalence in the Western world is shifting, with oropharyngeal cancer, a malignancy affecting the tonsils and back of the throat, experiencing a dramatic surge in recent decades, reaching epidemic proportions. Research led by Professor Hisham Mehanna at the University of Birmingham pinpoints the human papillomavirus (HPV), a sexually transmitted infection, as the primary driver of this alarming trend. While HPV is also recognized as the leading cause of cervical cancer, it has now surpassed cervical cancer in prevalence in both the US and the UK, highlighting the escalating threat of HPV-related oropharyngeal cancer. Specifically, the research identifies oral sex as the main mode of transmission for HPV in this context, establishing a clear link between sexual behavior and the increasing incidence of this cancer.
The study emphasizes the significance of the number of lifetime oral sex partners as a critical risk factor for developing oropharyngeal cancer. Individuals with a history of six or more oral sex partners are found to be 8.5 times more likely to develop the disease compared to those who have never engaged in oral sex. This finding underscores the direct correlation between oral sexual activity and HPV transmission, ultimately increasing the risk of oropharyngeal cancer. While oral sex is a common practice, with a reported 80% of adults in the UK having engaged in it at some point, only a small percentage develop oropharyngeal cancer. This discrepancy suggests that while the majority can successfully clear HPV infections, a vulnerable minority are unable to do so, potentially due to underlying immune system deficiencies, allowing the virus to persist and potentially trigger cancerous growth.
The current understanding of HPV-related carcinogenesis posits that the virus integrates into the host’s DNA, disrupting cellular processes and potentially leading to uncontrolled cell growth and tumor formation. The persistent presence of HPV in the oropharynx, facilitated by the inability of some individuals to clear the infection, creates a chronic inflammatory environment, further increasing the risk of malignant transformation. The link between oral sex, HPV infection, and oropharyngeal cancer emphasizes the importance of preventive measures, particularly focusing on vaccination and safe sexual practices.
Given the established link between HPV and oropharyngeal cancer, vaccination emerges as a crucial preventative strategy. Many countries have implemented HPV vaccination programs primarily targeting young girls to protect against cervical cancer. However, growing evidence highlights the effectiveness of these vaccines in preventing oral HPV infections, thereby offering protection against oropharyngeal cancer as well. This dual benefit of the HPV vaccine underscores its broader potential in combating HPV-related diseases, regardless of gender. Furthermore, the concept of herd immunity, where vaccination of a significant portion of the population indirectly protects unvaccinated individuals, has shown to benefit boys in regions with high vaccine coverage among girls. This observation further supports the rationale for extending HPV vaccination to boys, creating a more comprehensive and equitable approach to prevention.
Recognizing the broader protective benefits of the HPV vaccine, countries like the UK, Australia, and the US have expanded their vaccination recommendations to include young boys, adopting gender-neutral policies. This inclusive approach aims to maximize population-level protection against HPV-related cancers, recognizing the shared vulnerability of both genders to HPV infection and its potential consequences. However, despite the demonstrable benefits of universal vaccination, achieving full coverage remains a challenge. Vaccine hesitancy, fueled by safety concerns and misconceptions about promoting promiscuity, presents a significant barrier to widespread adoption. Furthermore, the COVID-19 pandemic has exacerbated these challenges, disrupting access to vaccination services and contributing to a rise in anti-vaccine sentiments.
Professor Mehanna’s findings underscore the urgent need for a multifaceted approach to address the growing threat of oropharyngeal cancer. Public health initiatives should focus on raising awareness about the link between oral sex, HPV, and oropharyngeal cancer, promoting safe sexual practices, and emphasizing the protective benefits of HPV vaccination for both genders. Combating vaccine hesitancy requires targeted communication strategies that address public concerns, dispel misinformation, and highlight the long-term health benefits of vaccination. Overcoming these challenges is crucial to effectively curb the rising incidence of oropharyngeal cancer and protect future generations from this increasingly prevalent malignancy. The shift in the cancer landscape, with oropharyngeal cancer surpassing cervical cancer in some regions, serves as a stark reminder of the evolving nature of health threats and the need for adaptable and proactive public health strategies.